Transcranial Magnetic Stimulation
Since its introduction in 1985,
researchers have used transcranial magnetic stimulation as a research tool to
gain many insights into the physiology of the brain. Now, increasing research
suggests that the technique, which uses a powerful electromagnet discharge to
alter brain activity, may also hold promise as a treatment. Research indicates
that those with depression and a variety of other brain illnesses may benefit.
Scientific American
Specifically, research indicates that powerful magnetic
fields used in a technique known as transcranial magnetic stimulation, or TMS,
can alter and sometimes aid brain activity. The findings are leading to:
- A
better understanding of the effect of magnetic fields on the brain.
- New
ideas on how to treat brain illnesses, such as depression.
Starting in 1985 researchers began to find evidence that
high-powered magnetic techniques create large effects. That year they
introduced TMS and found that its activation over a brain area involved in
movement stimulated brain activity and triggered muscle twitches.
At first scientists used TMS mainly as a research tool to
gain insights into how the brain works. But in recent years, scientists refined
the strategy and found evidence that it can change brain activity and sometimes
alleviate depression.
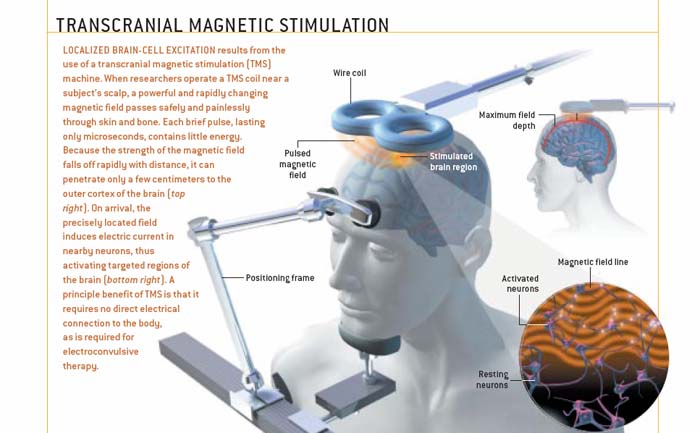
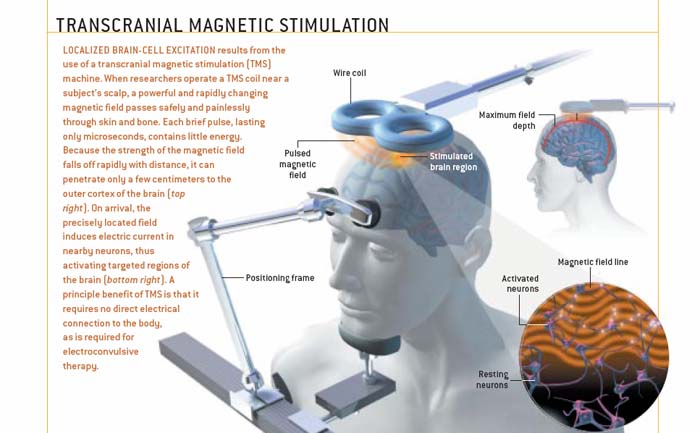
During current TMS sessions (see illustration) a researcher
holds an electromagnetic coil against the scalp. It produces almost painless
magnetic pulses that easily pass through the skull. These pulses then induce an
electric current that alters the activity of the brain's nerve cells.
Typically, for depression, the sessions last a half hour and occur each weekday
for two weeks.
Recently, several small studies show that compared to fake
stimulation, the TMS strategy improves the mood of people with depression
without causing any major side effects. A large study, designed to include more
than 85 depressed patients, is underway to confirm the benefits. Researchers
also are trying to unravel how it works to improve mood. Many believe that
depressed individuals have depressed activity in the front part of the brain,
and some speculate that TMS works by boosting this activity.
Researchers currently are comparing TMS in humans and animals
with another brain-altering therapy, electroconvulsive therapy or ECT, to
determine the most effective technique. Doctors often use ECT on severely
depressed patients who don't respond well to antidepressant medications. In
ECT, electrodes placed on the scalp trigger electrical stimulation of the
brain. But unlike the TMS treatment, which creates targeted activity, ECT
currents have trouble crossing the skull and create widespread brain
stimulation.
In other work, scientists are finding that additional brain
ailments may benefit from TMS. For example, researchers found that TMS applied
to the front part of the brain speeds up the ability of healthy volunteers to
solve puzzles requiring skills in analogical reasoning. Next, they plan to test
whether the technique can help reinstate lost abilities in patients with brain
disorders, such as Parkinson's disease and stroke.
New York Times
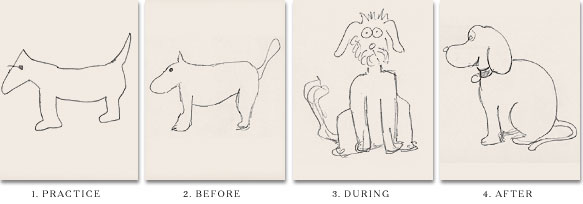
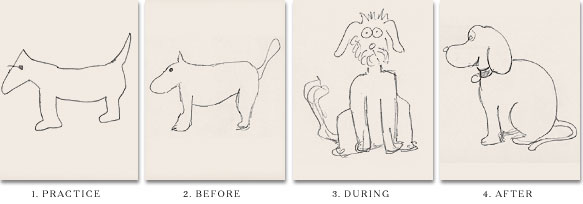
The research of a test in which a research subject was
asked to draw a picture of a
dog four times, at different stages of
his exposure to transcranial magnetic stimulation.
Some research also indicates that TMS tuned to emit a low
frequency force can reduce brain activity, which suggests that it may help
disorders tied to overactivity in the brain. Recently, one study examined the
effect of TMS on people who have the brain disorder, schizophrenia, and hear
imaginary voices. Directed at brain areas that process speech and may be
overactive in the patients, TMS muted the voices. In another example,
researchers tested TMS on patients with post-traumatic stress disorder. This
condition, marked by anxiety and depression, seems to involve high activity in
brain circuits involved in negative emotions. Low frequency TMS decreased the
activity in these circuits and improved symptoms.
With continued research, many scientists are confident that
magnetic stimulation will help treat these illnesses and many others.
Read Scientific American Article on
Magnetic Stimulation
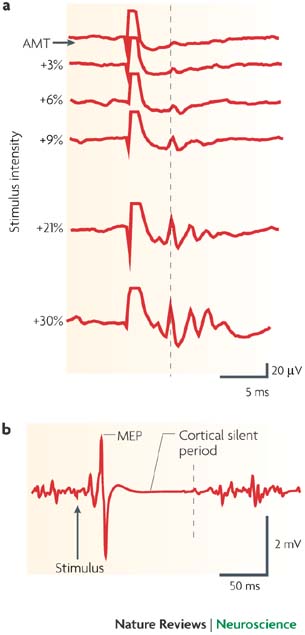
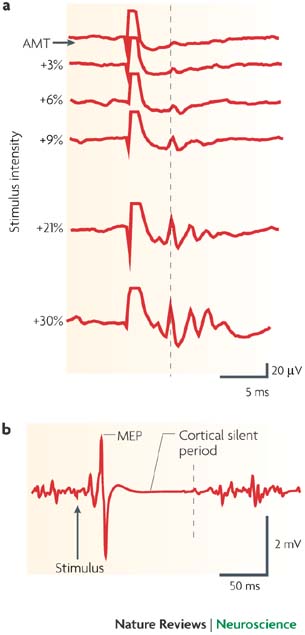
a | Descending volleys evoked by single-pulse
transcranial magnetic stimulation (TMS) recorded from the epidural space of
the cervical spinal cord in a conscious human subject. Stimulus intensities
ranged from active motor threshold (AMT) to AMT + 30% (of maximum stimulator
output). With increasing stimulus intensities a series of waves (I-waves) is
recruited that result from trans-synaptic (that is, indirect) activation of
corticospinal tract neurons. The first of these I-waves, termed I1, is
indicated by the dashed vertical line.
b | An electromyographic response that was
recorded while the subject was contracting a small hand muscle (first dorsal
interosseous) to a single pulse of TMS at an intensity of 110% resting motor
threshold. Approximately 20 ms after the stimulus is a large motor-evoked
potential (MEP), followed by a period of relative quiescence of background
EMG activity known as the 'cortical silent period'. The end of the silent
period is indicated by the dashed vertical line.
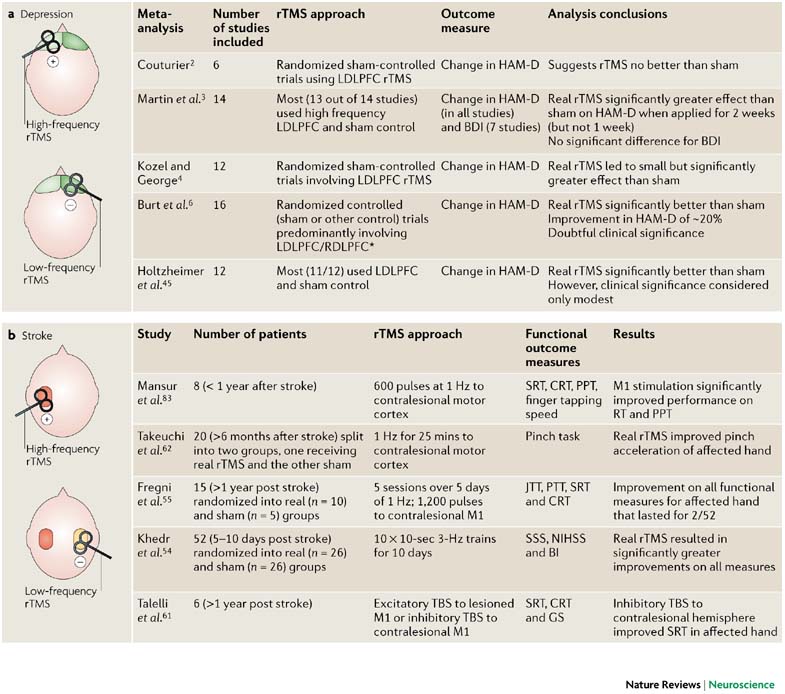
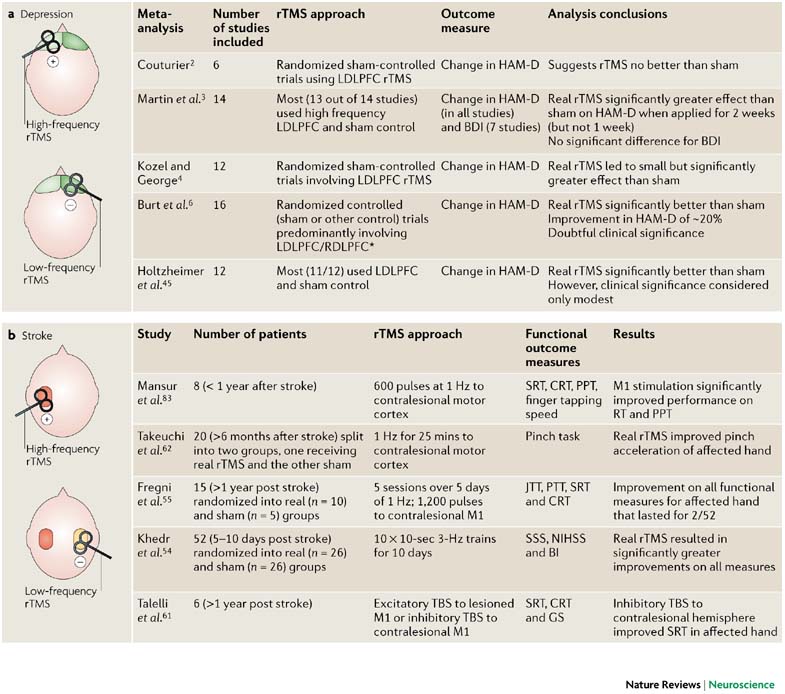
a | Schematic representation of two
different repetitive transcranial magnetic stimulation (rTMS) approaches
used in studies investigating the effect of rTMS on depression. In one
approach, high-frequency, excitatory rTMS is targeted to the hypoactive
(pale green) left prefrontal cortex (PFC). In the second approach,
low-frequency, inhibitory rTMS is directed at the hyperactive (bright
green) right PFC. The table summarizes results from a number of
meta-analyses that examined the use of rTMS in depression.
b | Schematic representation of the
different rTMS approaches used in studies investigating the effect of
rTMS on stroke. One approach applies high-frequency, excitatory rTMS to
the lesioned (red) hemisphere, whereas in the other approach low
frequency, inhibitory rTMS is targeted to the intact (yellow) hemisphere
to reduce its excitability. The table summarizes results from primary
studies that used rTMS protocols in stroke patients. BDI, Beck
depression inventory; BI, Barthel Index scale; CRT, choice reaction
time; GS, grip strength; HAM-D, Hamilton Rating Scale for Depression;
JTT, Jebson-Taylor hand function test; LDLPFC, left dorsolateral
prefrontal cortex; M1, motor cortex; NIHSS, National Institutes of
Health Stroke Scale; PPT, Purdue pegboard test; RDLPFC, right
dorsolateral prefrontal cortex ; RT, reaction time; SRT, simple reaction
time; SSS, Scandinavian Stroke Scale; TBS, theta-burst stimulation.
*Several studies in this meta-analysis involved stimulation of
other sites including the vertex, and the temporal and parietal cortices
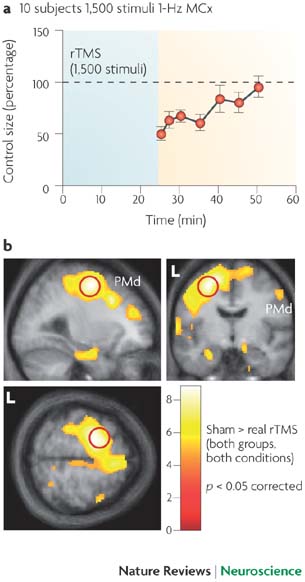
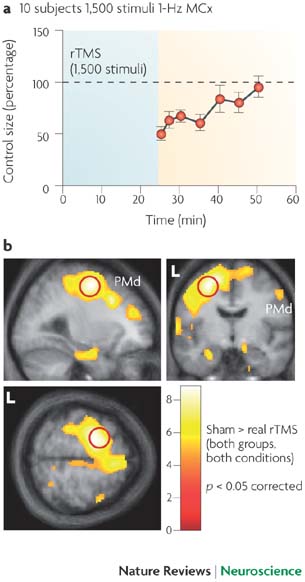
a | Time course of
changes in excitability of the motor cortex after 25
min reptitive transcranial magnetic stimulation (rTMS;
blue shading) at 1 Hz and an intensity of 90%
resting threshold. Data reflect the amplitude of the
electromyographic response to a single TMS pulse as
a percentage of the amplitude before rTMS. The
response is suppressed immediately after rTMS and
this effect persists to a decreasing extent for the
next 30 min.
b | Brain images
from a study that used positron emission tomography
(PET) to measure metabolic activity. The colour
coding shows the areas in which activity after a 25
min session of real 1-Hz rTMS over the dorsal
premotor cortex (PMd) is less than that seen after a
sham rTMS session. Numbers in the colour code bar
are Z-scores, which indicate the probability that
the activation differs from the rest; Z>4 is highly
significant. There are significant decreases in
activity after real rTMS at the site of stimulation
(outlined in red) as well as at many distant sites.
L, left side of the brain. Panel a
modified, with permission, from Ref.
10 © (2001) International Federation of Clinical
Neurophysiology. Panel b
modified, with permission, from Ref.
82 © (2003) Oxford Univ. Press.
Download
file
If the
slide opens in your browser, select "File >
Save As" to save it.